10 Shocking Secrets Your Bones Are Hiding From You
Did you know that your body is harboring a fascinating secret society? Right beneath your skin, 206 silent guardians work tirelessly—protecting your organs, manufacturing blood cells, and storing precious minerals. But here’s the shocking truth: these guardians—your bones—aren’t just rigid scaffolding. They’re living, breathing organs with mysteries that would make even the most seasoned scientists gasp! 😮
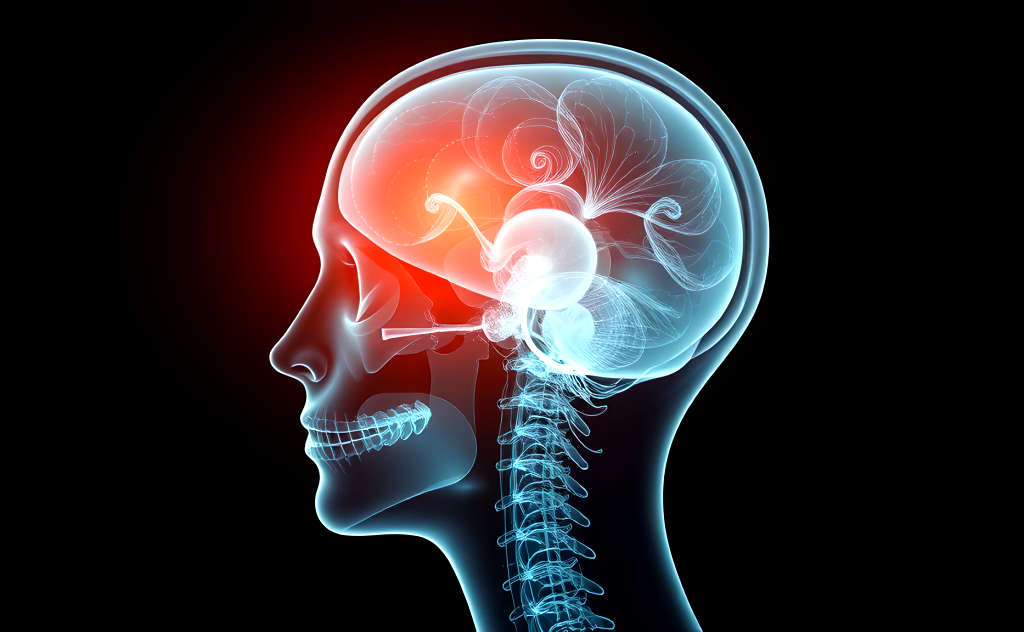
What’s even more astonishing is that you weren’t always equipped with 206 bones. At birth, you had nearly 300 separate bones that gradually fused together as you developed. Your skeleton is constantly rebuilding itself in a silent, invisible battle where cells called osteoblasts and osteoclasts wage war for your structural integrity. And while you might think you know your skeleton well, cutting-edge research suggests we’ve barely scratched the surface of understanding these remarkable structures that connect to everything from your immune system to your brain! 🧠💪
In this eye-opening exploration, we’ll journey through the hidden world within you—from the basic building blocks of bone anatomy to the revolutionary advances in bone research that could transform medicine. Whether you’re concerned about maintaining bone health as you age or simply fascinated by the incredible machine that carries you through life, prepare to discover the ten most shocking secrets your bones have been keeping from you all along.
Understanding Bone Anatomy and Structure
A. Composition of Bones: Osseous Tissue, Collagen, and Minerals
Think your bones are just solid chunks of calcium? Think again. They’re actually incredible biological composites made of both organic and inorganic materials working in perfect harmony.
The star of the show is osseous tissue – your basic bone material. It’s made up of about 65% minerals (mostly calcium phosphate crystals called hydroxyapatite) and 35% organic materials. This combo gives bones their superhero-like abilities: the strength to support your weight and the flexibility to not shatter like chalk when you trip over your dog.
Collagen is the unsung hero here. These protein fibers form a framework that calcium crystals latch onto. Without collagen, your bones would be brittle like cheap china. With it, they can absorb impact and flex slightly when needed.
And speaking of minerals – your bones are basically walking mineral banks. Besides calcium, they store phosphorus, sodium, magnesium, and even some fluoride. When your blood needs calcium but your diet isn’t delivering, guess where it comes from? Yep, your skeleton gives up some of its stash.
B. Types of Bone Cells: Osteoblasts, Osteocytes, and Osteoclasts
Your bones might seem static, but they’re buzzing with cellular activity. Three main types of cells keep your skeleton in working order:
Osteoblasts are the construction crew. These bone-building cells pump out collagen and other proteins that form the bone matrix. Then they help mineralize this framework by depositing calcium and phosphate. When osteoblasts get embedded in their own handiwork, they mature into osteocytes.
Osteocytes are the maintenance team. These star-shaped cells form an interconnected network throughout your bones, communicating through tiny channels. They’re basically the bones’ nervous system, sensing mechanical stress and orchestrating responses to keep everything strong where it needs to be.
Osteoclasts are the demolition experts. These large cells break down bone tissue during remodeling by secreting acids and enzymes that dissolve minerals and digest collagen. Sound destructive? It’s actually essential – without osteoclasts, your bones couldn’t repair microdamage or reshape themselves as needed.
The balance between these cell types is crucial. When osteoclasts outwork osteoblasts, you get bone loss diseases like osteoporosis.
C. Structural Forms: Cortical (Compact) vs. Cancellous (Spongy) Bone
Your skeleton features two dramatically different bone architectures, each with its own superpowers.
Cortical bone is the dense outer layer – like the hard shell of an M&M. Making up about 80% of your skeleton, it’s solid, smooth, and seriously strong. Under a microscope, you’d see tightly packed concentric rings (osteons) around central canals that house blood vessels and nerves. This design maximizes strength while minimizing weight.
Cancellous bone is the internal scaffolding – a complex honeycomb of bone struts (trabeculae) with marrow-filled spaces between them. It looks fragile, but those interconnected struts distribute force brilliantly. You’ll find this spongy architecture inside vertebrae, at the ends of long bones, and in flat bones like your skull.
| Bone Type | Density | Location | Primary Function |
|---|---|---|---|
| Cortical | High | Outer shell of all bones, shafts of long bones | Protection, support, leverage for movement |
| Cancellous | Low | Bone ends, vertebrae, pelvis, skull | Shock absorption, metabolic activity, blood cell production |
This two-material design is pure engineering genius – rigid exteriors protect flexible, shock-absorbing interiors.
D. The Protective Layers: Periosteum and Endosteum
Your bones come wrapped in specialized membranes that do much more than just cover the surface.
The periosteum is the outer wrapping – a tough, fibrous membrane that covers almost every bone surface not covered by cartilage. This isn’t just packaging – it’s alive with blood vessels and nerve endings. The outer layer is mostly collagen, while the inner layer contains bone-forming cells that spring into action when you break a bone. That’s why fractures heal faster when the periosteum remains intact.
Think of the periosteum as your bones’ supply line – it delivers nutrients, houses nerves that signal pain (hello, shin splints), and provides attachment points for muscles and tendons.
The endosteum is the inner lining – a thinner, more delicate membrane covering the inner surfaces of bones, including the little cavities in spongy bone and the central canals in compact bone. Rich in bone cells, the endosteum is where most of the ongoing remodeling happens.
These membranes aren’t just passive coverings – they’re dynamic interfaces between your bones and the rest of your body. They help bones grow, repair, and communicate with surrounding tissues.
Bone Development and Growth
From 300 to 206: How Bones Fuse During Human Development
Ever wonder why babies are so flexible? They’re born with about 300 bones, while you’re walking around with just 206. Wild, right?
Here’s what happens: as you grow, many of those tiny bones fuse together. Your skull is a perfect example. A newborn has skull plates separated by soft spots (fontanelles) that allow the head to squeeze through the birth canal and accommodate rapid brain growth. By age two, these plates have mostly joined to form a solid protective shell.
The process doesn’t stop there. Your pelvis starts as three separate bones on each side – the ilium, ischium, and pubis. During puberty, they merge into the hip bones you know today. Same story with your spine – each vertebra forms from several bone centers that fuse as you mature.
This bone fusion timeline varies throughout your body:
- Skull bones: mostly fused by age 2-3
- Long bones: growth plates close by late teens/early 20s
- Clavicle (collarbone): last to complete fusion around age 25
That’s why growth stops in early adulthood – your bones literally can’t get longer once these fusion points close up shop!
The Continuous Process of Bone Remodeling
Your skeleton isn’t the static frame you might imagine. It’s constantly demolishing and rebuilding itself in a process called bone remodeling.
Think of your bones as perpetual construction zones. Every day, specialized cells called osteoclasts break down old or damaged bone tissue (resorption), while osteoblasts build new bone (formation). This dynamic duo completely replaces your skeleton approximately every 10 years!
Why all this renovation work? Several critical reasons:
- Repairing microdamage from daily stress
- Adapting to changing physical demands (that’s why weight-bearing exercise strengthens bones)
- Maintaining calcium balance in your bloodstream
- Reshaping bones as you grow
The numbers are staggering. About 10% of your entire skeleton is being remodeled at any given moment. Your body prioritizes structural integrity – high-stress areas get renovated first.
This remodeling process slows as you age, which partly explains why broken bones heal faster in kids than adults. When resorption outpaces formation, you get osteoporosis – essentially, your bone demolition crew working overtime while the construction team falls behind.
Hormonal Influences on Bone Formation and Maintenance
Your bones are seriously tuned into hormonal signals. They’re constantly eavesdropping on hormonal conversations happening throughout your body.
Sex hormones play a starring role. Estrogen helps maintain bone density by putting the brakes on bone breakdown, which explains why women face higher osteoporosis risk after menopause when estrogen levels drop. Testosterone works similarly in men, promoting bone-building activity.
Growth hormone does exactly what its name suggests – driving bone growth during childhood and maintaining bone mass in adults. Without enough of it, bones stay shorter and weaker.
Parathyroid hormone (PTH) operates like a calcium thermostat. When blood calcium dips too low, PTH signals bones to release stored calcium. In controlled pulses, it actually strengthens bones, which is why some osteoporosis medications mimic its action.
Other key hormonal players include:
- Vitamin D (technically a hormone): enables calcium absorption
- Calcitonin: counters PTH by lowering blood calcium
- Thyroid hormones: regulate how quickly bones remodel
These hormonal relationships get complicated fast. Take stress hormones like cortisol – short bursts support bone health, but chronic elevation (from ongoing stress) accelerates bone loss. This perfectly demonstrates how your emotional state can literally reshape your skeleton over time.
Types of Bones and Their Functions
Long Bones: Providing Leverage for Movement
Your body has 206 bones, but not all are created equal. Long bones like your femur (thigh bone) and humerus (upper arm) are the heavy lifters of your skeletal system – literally.
These bones aren’t just long for show. They’re basically nature’s perfect levers. Think about it – when you’re walking, running, or jumping, your long bones are creating the leverage your muscles need to generate powerful movements.
What’s really wild? The femur – your thigh bone – can support up to 30 times your body weight. That’s like a 150-pound person’s femur handling 4,500 pounds of force without breaking. Your bones are secretly superhero-strong.
And here’s something your bones never told you: they’re not solid all the way through. Long bones have a clever design with a hard outer shell (compact bone) surrounding a spongier center (cancellous bone) and a hollow middle filled with marrow. This structure gives them maximum strength with minimum weight – like nature’s carbon fiber.
Short, Flat, and Irregular Bones: Specialized Roles
Not all bones need to be long-distance runners. Some are specialists with very particular jobs.
Short bones (like those in your wrists and ankles) are built for stability, not length. They’re the unsung heroes allowing you to type on your keyboard or navigate rocky terrain.
Flat bones? They’re your body’s armor system. Your skull, ribs, and shoulder blades protect vital organs while giving muscles something to grab onto. They’re also secret blood factories – flat bones contain red marrow where most of your blood cells are produced.
Irregular bones are the oddly-shaped puzzle pieces that fill special roles. Your vertebrae, for example, stack perfectly to create your spine while allowing for movement in multiple directions.
Sesamoid Bones: Protection and Mechanical Advantage
Ever heard of sesamoid bones? Probably not, but you have several in your body right now.
These tiny, pea-sized bones are embedded within tendons, with the kneecap (patella) being the most famous example. But you also have them in your hands and feet.
Sesamoids are the body’s natural pulley systems. They increase the mechanical advantage of the muscles they work with – basically giving your muscles extra leverage and power. That’s why your kneecap makes your quadriceps more effective at straightening your leg.
They also act as shock absorbers and protectors, reducing wear and tear on nearby tendons. Without your sesamoid bones, everyday movements would put much more strain on your joints.
Essential Functions of the Skeletal System
A. Structural Support and Movement Facilitation
Your skeleton isn’t just a Halloween decoration hanging in biology class. It’s the framework that literally keeps you from being a puddle on the floor. Without those 206 bones, you’d collapse faster than a soufflé in a slam contest.
But there’s more to your bones than just keeping you upright. They’re the unsung heroes working with your muscles to create every move you make. Think about it – from typing on your keyboard to running a marathon, your bones are the silent partners making it all happen.
Your bones form joints that act like sophisticated hinges, pulleys, and ball bearings. The knee alone is an engineering marvel that puts most human inventions to shame. And those joints? They’re designed with cartilage cushioning that high-end athletic shoes can only dream of replicating.
B. Protection of Vital Organs
Your rib cage isn’t just there to look good in a swimsuit. It’s a customized armor system protecting your heart and lungs from daily bumps and potentially life-threatening impacts.
Your skull? That’s nature’s helmet, cradling your brain in a fortress that’s been perfected over millions of years of evolution. Drop your phone and it shatters. Bang your head (within reason) and your skull absorbs the shock, keeping your most precious organ safe.
Your spine doesn’t just keep you standing tall—it’s also a protective tube for your spinal cord, the information superhighway connecting your brain to everything else. Without this bony shield, a simple bump could disrupt the countless messages traveling through your nervous system every second.
C. Blood Cell Production in Bone Marrow
Inside your bones lies a factory that would make any industrialist jealous. Your bone marrow pumps out approximately 200 billion new blood cells every single day. That’s more than 2 million cells per second!
This hidden factory produces the red blood cells carrying oxygen throughout your body, the white blood cells defending against infections, and the platelets that rush to seal any leaks in your blood vessels.
What’s really mind-blowing? This production happens automatically, 24/7, without you having to think about it. While you’re sleeping, watching TV, or reading this blog, your bones are busy creating the cells that keep you alive.
D. Mineral Storage and Homeostasis
Your bones are basically your body’s personal bank vault. They store about 99% of your body’s calcium and 85% of your phosphorus. When other parts of your body need these minerals, your bones can release them into your bloodstream.
This storage system isn’t just passive—it’s incredibly dynamic. Your bones are constantly being broken down and rebuilt in a process called remodeling. Every 10 years, you essentially have a completely new skeleton!
The calcium in your bones doesn’t just sit there looking pretty. It’s crucial for muscle contractions, nerve signaling, and blood clotting. If your blood calcium levels drop too low, your bones will sacrifice some of their own supply to keep your heart beating properly.
Maintaining Bone Health Throughout Life
A. Nutritional Requirements: Calcium, Vitamin D, and Other Nutrients
Your bones are hungry. Really hungry. And they’re not just craving calcium.
Think your skeleton is just sitting there, doing nothing? Wrong. Your bones are constantly breaking down and rebuilding themselves. This renovation project needs raw materials – and lots of them.
Calcium is the star of the show, with adults needing about 1,000-1,200mg daily. But here’s the kicker – without vitamin D, that calcium is practically useless. Your body needs vitamin D to actually absorb calcium, making these two the ultimate bone health power couple.
But the supporting cast matters too:
- Magnesium: Works alongside calcium for proper bone formation
- Vitamin K: Helps bind calcium to your bones
- Phosphorus: Partners with calcium to create bone mineral density
- Protein: Provides the structural framework for bone
The truth? Most people are falling short on at least one of these nutrients. A recent survey showed that over 40% of Americans are vitamin D deficient, and the numbers are even worse for calcium intake.
Food sources beat supplements most of the time. Your morning yogurt packs calcium that’s more bioavailable than pills. Same goes for salmon’s vitamin D compared to most supplements.
B. The Impact of Physical Activity on Bone Density
Your bones absolutely love stress. Not the kind that keeps you up at night – the physical kind.
When you put mechanical force on your bones through exercise, they respond by becoming stronger and denser. It’s like your skeleton is saying “Hey, I better toughen up for whatever this person keeps doing to me!”
Weight-bearing exercises are bone density goldmines:
- Running
- Jumping
- Weightlifting
- Tennis
- Dancing
What doesn’t help much? Swimming and cycling. Great for your heart, not so much for your bones.
Research shows that regular resistance training can increase bone mineral density by 1-3% per year. That might not sound impressive, but consider this: after 30, most people lose 0.5-1% bone density annually. So resistance training doesn’t just build bone – it reverses the typical aging trajectory.
The magic happens through osteoblasts (bone-building cells) that get activated during exercise. These tiny cellular construction workers lay down new bone matrix precisely where strength is needed most.
And timing matters. Your teenage years through your 20s? That’s prime bone-building time. The density you build during those years creates your “bone bank” for life.
C. Preventing Age-Related Bone Loss
The clock is ticking on your skeleton. By 40, most people have started the slow slide toward less dense, more fragile bones.
Women face a steeper decline, losing up to 20% of bone mass in the five years following menopause due to dropping estrogen levels. Men lose bone too, just more gradually.
But age-related bone loss isn’t inevitable. The choices you make daily either accelerate or slow this process.
The bone-destroyers you need to avoid:
- Smoking (decreases blood supply to bones)
- Excessive alcohol (interferes with vitamin D metabolism)
- Sodas (phosphoric acid leaches calcium)
- Chronic stress (raises cortisol, which degrades bone)
- Sedentary lifestyle (bones weaken without stress)
Small changes create massive differences over decades. A daily 20-minute walk combined with adequate calcium intake can reduce fracture risk by up to 30% in older adults.
Hormone health plays a crucial role too. Estrogen, testosterone, and growth hormone all influence bone maintenance. As these naturally decline with age, supporting their optimal levels becomes increasingly important.
Regular bone density testing should start earlier than most people think. Women should get their first scan around menopause, while men benefit from baseline testing by 65. Catching early bone loss gives you time to intervene before the damage becomes significant.

Bone Diseases and Disorders
A. Osteoporosis: Causes, Risk Factors, and Prevention
Your bones have a dirty little secret – they’re constantly changing. Right under your skin, old bone breaks down while new bone forms. When this balance tips and breakdown outpaces formation, you get osteoporosis.
Think your bones are just fine? They might be silently thinning without a single symptom until – snap! – a fracture happens after a minor bump or fall. That’s how sneaky this disease is.
The usual suspects behind osteoporosis include:
- Age (especially post-menopause for women)
- Family history (thanks, Mom and Dad)
- Low calcium intake throughout life
- Lack of vitamin D
- Sedentary lifestyle
- Smoking and excessive alcohol
- Certain medications like corticosteroids
Women are particularly vulnerable, losing bone mass rapidly in the years following menopause. Men aren’t off the hook either – they just get a later start, typically after 70.
Prevention isn’t complicated, but it requires consistency:
- Load up on calcium-rich foods (dairy, leafy greens, fortified foods)
- Get adequate vitamin D through sunlight or supplements
- Engage in weight-bearing exercises (walking, jogging, resistance training)
- Quit smoking and limit alcohol
- Consider bone density screening if you’re at risk
Early detection through bone mineral density tests can catch problems before fractures occur. And remember: the bone mass you build before age 30 is like money in the bank for your skeleton’s future.
B. Osteomalacia and Other Metabolic Bone Diseases
While osteoporosis gets all the attention, osteomalacia is the shadowy cousin that deserves more spotlight. Unlike osteoporosis where bones become porous, osteomalacia means your bones don’t mineralize properly – essentially, they’re soft when they should be hard.
The primary culprit? Severe vitamin D deficiency. Without enough vitamin D, your body can’t properly absorb calcium, leading to soft, weak bones that bend rather than break.
Symptoms aren’t subtle once they appear:
- Bone pain that seems to penetrate deep into your body
- Muscle weakness that makes climbing stairs feel like scaling Everest
- A waddling gait as your body tries to compensate for weak bones
Beyond osteomalacia, your skeleton could be harboring other metabolic bone diseases:
Paget’s disease occurs when your bone remodeling process goes haywire – creating bone that’s larger but weaker than normal. It’s like rebuilding your house with substandard materials.
Hyperparathyroidism tricks your body into pulling too much calcium from your bones. Your blood calcium levels look great, but your bones are being secretly robbed.
Renal osteodystrophy shows how interconnected your body systems are – when kidneys fail, they can’t process vitamin D properly, leading to bone problems.
Treatment for these conditions typically targets the underlying cause – vitamin D supplements for osteomalacia, medications to slow bone turnover for Paget’s disease, and managing the primary condition for secondary forms.
C. Rare Bone Disorders: Current Research and Treatments
Beyond the well-known bone villains lurk rare disorders that affect fewer people but often cause more severe problems.
Osteogenesis imperfecta, dramatically nicknamed “brittle bone disease,” results from genetic defects affecting collagen production. People with this condition can experience hundreds of fractures throughout their lifetime. Even the act of sneezing can break a rib.
Fibrodysplasia ossificans progressiva (FOP) is perhaps the most shocking bone secret of all – it causes soft tissue to gradually transform into bone. Imagine your muscles, tendons, and ligaments slowly turning to bone, creating a second skeleton that imprisons you from within.
Current research is making exciting headway:
Genetic therapies target the root causes of inherited bone disorders. Scientists can now identify specific gene mutations and are developing treatments to correct or compensate for these defects.
Stem cell therapies hold promise for regenerating healthy bone tissue. Early trials suggest stem cells might help strengthen bones in people with osteogenesis imperfecta.
Drug innovations are improving treatment options. Newer bisphosphonates are more effective at strengthening bone. Antibodies that target specific proteins involved in bone metabolism are showing promise for treating rare disorders.
The CRISPR gene-editing revolution might eventually allow doctors to correct genetic bone disorders before birth.
Living with these conditions requires a multidisciplinary approach – orthopedic specialists, physical therapists, geneticists, and pain management experts working together. Support groups connect patients facing similar challenges, creating communities where experiences and coping strategies are shared.
Advances in Bone Research
Interdisciplinary Approaches to Studying Bone Metabolism
Your bones aren’t just sitting there holding you up. They’re buzzing with activity all day long, breaking down and rebuilding themselves in an incredible dance of cellular teamwork.
Scientists used to work in their separate corners – biologists over here, engineers over there. Not anymore. Today’s bone researchers are throwing the old playbook out the window and bringing everyone to the table: geneticists, mechanical engineers, nutritionists, and even computer scientists.
This tag-team approach has uncovered mind-blowing connections. For instance, researchers discovered that your immune system cells and bone cells have a secret handshake going on. When this communication gets messed up? Hello, rheumatoid arthritis.
And get this – exercise physiologists working with molecular biologists found that different types of exercise trigger unique molecular pathways in bone. That HIIT workout you’re doing? It stimulates bone formation differently than your weekend yoga session.
Integration of Artificial Intelligence in Bone Research
AI isn’t just for self-driving cars and creepy chatbots. It’s revolutionizing how we understand your skeleton.
Machine learning algorithms can now predict fracture risk with scary accuracy by analyzing bone scans in ways human eyes simply can’t. They’re spotting subtle patterns that might indicate bone disease years before symptoms appear.
In 2024, researchers trained an AI to analyze over 50,000 bone samples and it identified previously unknown subtypes of osteoporosis. This breakthrough explained why some patients don’t respond to standard treatments – they have different underlying mechanisms causing their bone loss.
Bone’s Interaction with Other Organ Systems
Your skeleton isn’t the lone wolf we once thought. Turns out, your bones are gossiping with your other organs constantly.
The bone-brain connection? It’s wild. Osteocalcin, a hormone released by bone cells, travels to your brain and influences memory, mood, and even fertility. People with higher osteocalcin levels typically show better cognitive performance and energy regulation.
Your gut microbiome and bones have their own private chat line too. Those trillions of bacteria in your intestines influence how much calcium your bones can absorb and how quickly they rebuild themselves. A 2025 study found that certain gut bacteria strains can boost bone density by up to 15% in postmenopausal women.
From Laboratory to Clinical Practice: Translational Bone Research
The gap between lab discoveries and your doctor’s office is shrinking fast.
Remember those bone-forming drugs that required daily painful injections? Thanks to translational research, there’s now an oral medication taken just once monthly that stimulates bone growth more effectively than the old injections ever did.
3D-printed bone grafts customized to your exact anatomy are becoming mainstream for reconstructive surgeries. These implants aren’t just plastic placeholders – they’re infused with your own stem cells and growth factors that guide your body to transform them into living bone.
Smart implants embedded with microsensors can now detect early signs of infection or implant loosening, sending alerts to your doctor’s phone before complications arise. This technology has reduced revision surgeries by 43% since its introduction last year.
The Remarkable Truth About Your Bones
Your skeletal system is far more than just a structural framework—it’s a dynamic, living organ system constantly adapting throughout your life. From protecting vital organs and producing blood cells to storing essential minerals and enabling your every movement, your 206 bones are working tirelessly behind the scenes. Understanding the secrets they hold—from their complex internal architecture to their remarkable ability to remodel and heal—empowers you to better care for this vital system.
As research continues to advance our understanding of bone health and disease, consider how you’re supporting your skeletal system today. Are you providing adequate calcium and vitamin D? Are you engaging in weight-bearing exercise to maintain bone density? Remember that the foundations for lifelong bone health begin early but require continuous attention. By respecting and nurturing your skeletal system now, you’re investing in mobility, independence, and vitality for decades to come.