Finding Balance: The Key to Women’s Hormonal Health
Have you ever experienced unexplained weight fluctuations, persistent fatigue, or mood swings that seem to come out of nowhere? For millions of women, these aren’t just random occurrences—they’re potential signs of hormone imbalance. As the body’s chemical messengers, hormones orchestrate everything from your metabolism and mood to reproductive functions and sleep patterns. When these delicate messengers fall out of balance, the effects can ripple through virtually every aspect of your wellbeing, impacting not just how you feel physically, but your emotional state and quality of life too.
The female body is particularly susceptible to hormonal shifts, with natural fluctuations occurring throughout life stages like menstruation, pregnancy, and menopause. But when these chemical messengers veer too far from their optimal levels—whether from stress, medications, or underlying health conditions—the consequences can be far-reaching. From chronic acne and irregular periods to sleep disturbances and cognitive fog, hormone imbalances manifest in surprisingly diverse ways that many women mistakenly attribute to aging, stress, or “just life.” The good news? Most hormone-related conditions can be effectively managed or treated once properly identified. 💪
In this comprehensive guide, we’ll explore the intricate world of female hormones—unpacking their essential functions, recognizing imbalance symptoms, examining common hormone-related conditions, and most importantly, discovering proven strategies to restore and maintain optimal hormone health naturally. Whether you’re navigating the challenges of perimenopause or simply seeking to understand your body better, this roadmap to hormone balance will empower you with the knowledge to take control of your hormonal health.
Understanding Female Hormones and Their Vital Functions
The Role of Hormones as Chemical Messengers in the Body
Think of your body as a bustling city, with millions of cells needing to communicate with each other constantly. That’s where hormones come in – they’re like the text messages your organs send to each other.
These powerful chemical messengers travel through your bloodstream, telling your body what to do and when to do it. They control everything from your mood and energy levels to your reproductive cycle and metabolism.
What makes hormones so fascinating is how tiny amounts can trigger massive changes. Just a few molecules of estrogen can signal your ovaries to release an egg, while a splash of cortisol can prepare your entire body for a fight-or-flight response.
Unlike the nervous system which sends immediate electrical signals, hormones work on a slower timeline – sometimes taking hours or days to create their effects. This is why hormonal shifts don’t happen instantly but unfold gradually.
How the Endocrine System Regulates Hormone Production
Your endocrine system is the command center for hormone production. It’s a network of glands scattered throughout your body, each responsible for creating specific hormones.
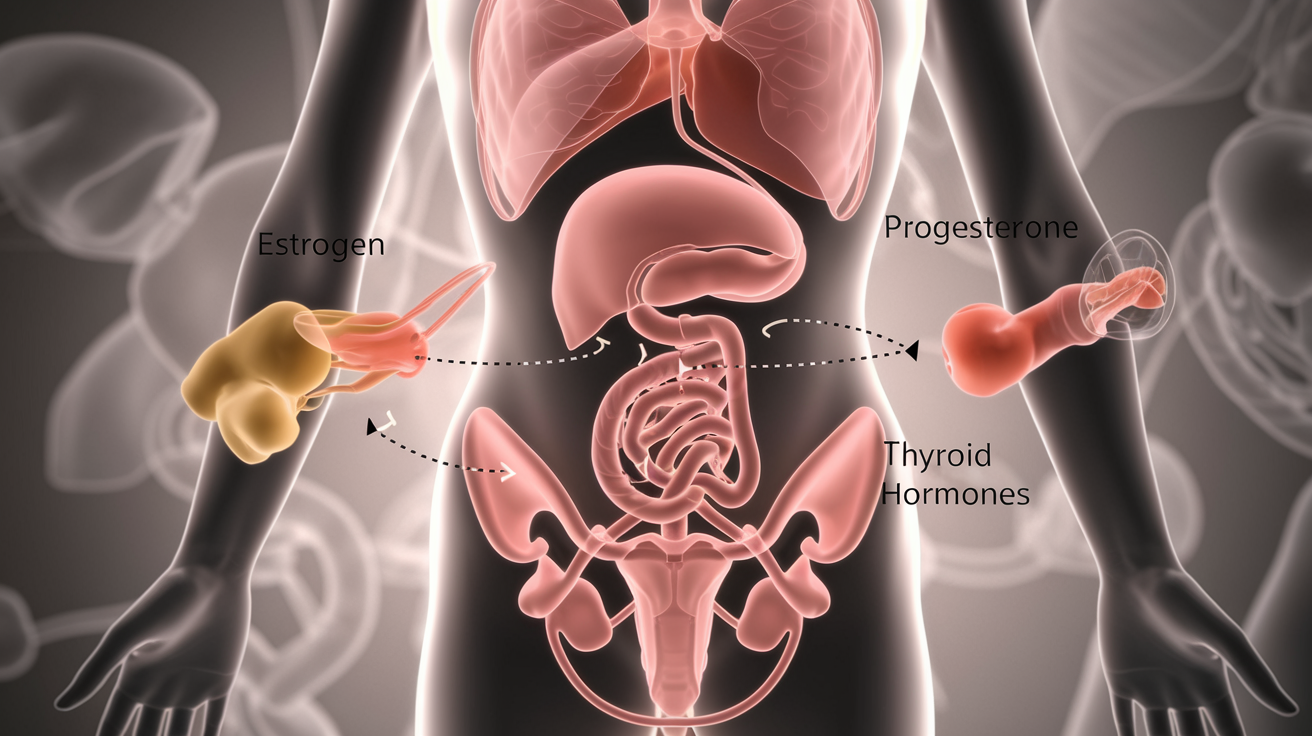
The main players include:
- Pituitary gland: The “master gland” that directs other glands
- Ovaries: Produce estrogen and progesterone
- Thyroid: Controls metabolism and energy
- Adrenal glands: Make stress hormones like cortisol
- Pancreas: Regulates blood sugar with insulin
These glands don’t just randomly pump out hormones. They use a sophisticated feedback system – like a thermostat that maintains the perfect temperature in your home. When hormone levels rise too high, production slows down. When they drop too low, production ramps up.
This delicate balancing act happens constantly, but sometimes the system gets thrown off by stress, poor nutrition, environmental toxins, or aging.
Key Hormones Affecting Women’s Health and Wellbeing
Women’s bodies rely on several critical hormones that dramatically influence health, mood, and quality of life:
Estrogen: Far more than just a reproductive hormone, estrogen affects your brain, bones, heart, skin and mood. It gives you energy, keeps your skin plump, and protects your bone density. During perimenopause, its fluctuations can trigger hot flashes and mood swings.
Progesterone: The calming counterpart to estrogen, progesterone helps you sleep, reduces anxiety, and prepares your uterus for pregnancy. When it’s low, you might experience insomnia, irritability, and heavy periods.
Testosterone: Yes, women need this “male” hormone too! It drives your libido, helps maintain muscle mass, and contributes to confidence and motivation. Many women notice its decline during their 40s.
Thyroid hormones: These metabolism regulators affect everything from your weight and energy to your hair and digestion. Women are five times more likely than men to develop thyroid problems.
Cortisol: Your primary stress hormone helps you respond to challenges, but chronic elevation can disrupt sleep, increase belly fat, and suppress your immune system.
The complex dance between these hormones creates your unique biochemical environment. When they’re in harmony, you feel energetic, emotionally balanced, and healthy. When they’re out of sync, your body lets you know through various symptoms.
Recognizing Signs of Hormone Imbalance in Women

Physical Symptoms: Weight Fluctuations, Fatigue, and Skin Changes
Ever notice how your body sometimes seems to have a mind of its own? That’s your hormones talking. When they’re out of whack, your body sends pretty clear signals.
Weight gain that shows up overnight (especially around your middle) isn’t always about that extra slice of pizza. Hormonal imbalances, particularly with insulin, cortisol, or estrogen, can make your body cling to fat like it’s going out of style. And the frustrating part? Even your usual workout routine might suddenly stop working.
Feeling like you need three naps a day? Chronic fatigue isn’t just about needing more coffee. When your thyroid hormones drop too low, it’s like someone unplugged your body’s energy supply. Meanwhile, cortisol imbalances from stress can leave you wired at night but completely drained during the day.
Your skin tells hormone stories too. Sudden acne breakouts (yes, even in your 30s and 40s) often point to excess androgens. Dry, thinning skin? That might be low estrogen talking. And those dark patches appearing on your cheeks and forehead (melasma)? Blame hormone fluctuations, especially during pregnancy or when taking birth control.
Emotional and Cognitive Signs: Mood Swings, Memory Issues, and Sleep Disturbances
Your brain is basically a hormone playground. When the playground rules get messy, so does your emotional state.
Those days when you’re crying at commercials one minute and snapping at your partner the next? Classic signs of estrogen and progesterone imbalance. These mood swings aren’t character flaws – they’re chemical reactions happening in your body that feel completely beyond your control.
Brain fog isn’t just a cute term for forgetfulness. When women complain about forgetting words mid-sentence or walking into rooms with no clue why they’re there, hormones are often the culprits. Estrogen actually helps with cognitive function, so when levels drop (hello, perimenopause), your mental clarity can take a hit.
Sleep problems are particularly sneaky hormone signs. Having trouble falling asleep? Cortisol might be running high when it should be winding down. Waking up at 3am for no reason? Low progesterone could be the midnight party-crasher. And those night sweats that leave you drenched? Estrogen fluctuations love to mess with your body’s temperature regulation.
Reproductive and Sexual Health Indicators: Menstrual Irregularities and Libido Changes
Your period is basically a monthly hormone report card. When it starts behaving strangely, your body’s trying to tell you something important.
Periods that suddenly become heavier, lighter, more painful, or decide to take random vacations point to hormone imbalances. Estrogen and progesterone need to dance together in a specific rhythm – when one leads too strongly or doesn’t show up at all, your cycle gets the message loud and clear.
PMS that feels like it’s taken over your life might indicate excess estrogen relative to progesterone. And if you’re dealing with PCOS, your irregular periods come with a side of excess androgens, creating a frustrating hormone cocktail.
Your sex drive isn’t just about relationship satisfaction – it’s deeply connected to your hormone health. Low libido often accompanies drops in estrogen and testosterone (yes, women need testosterone too!). Meanwhile, vaginal dryness that makes intimacy uncomfortable typically points to declining estrogen, particularly during perimenopause and menopause.
The connection between painful sex and hormones is real and deserves attention. Many women suffer silently, not realizing that hormone therapy might offer relief from issues like thinning vaginal tissues and decreased natural lubrication.
Common Hormone-Related Conditions Women Experience

Thyroid Disorders and Their Impact on Metabolism
Your thyroid is like the gas pedal for your entire body. When it’s off, everything feels off.
Women are 5-8 times more likely than men to develop thyroid issues. And the symptoms? They’re sneaky. Unexplained weight changes, feeling cold all the time, brain fog, fatigue that coffee can’t fix… sound familiar?
The two main culprits are:
-
Hypothyroidism: Your thyroid’s moving too slow, and so are you. Your metabolism crawls, you gain weight despite eating the same, and you might feel depressed or sluggish.
-
Hyperthyroidism: The opposite problem – your thyroid’s working overtime. You might lose weight mysteriously, feel anxious, have heart palpitations, or sweat through nights.
Many women walk around with undiagnosed thyroid conditions for years, blaming themselves for symptoms that have a biological cause.
Reproductive Health Issues: PCOS, Endometriosis, and Infertility
These aren’t just “women’s problems” – they’re serious hormone-driven conditions affecting millions.
PCOS (Polycystic Ovary Syndrome) impacts about 1 in 10 women. The hallmarks? Irregular periods, excess androgens (hello, unwanted hair and acne), and those infamous ovarian cysts. Behind it all: a hormone imbalance that often involves insulin resistance.
Endometriosis affects roughly the same number of women. Picture tissue similar to your uterine lining growing where it shouldn’t – on your ovaries, fallopian tubes, and elsewhere in your pelvis. The result? Often debilitating pain and potential fertility challenges.
Both conditions can contribute to infertility, which impacts about 15% of couples. The hormone connection is clear – without the right balance and timing of estrogen, progesterone, LH, and FSH, conception becomes an uphill battle.
What’s worse? The average diagnosis time for these conditions is measured in years, not months.
Age-Related Hormonal Shifts: Perimenopause and Menopause
Nobody talks about the hormonal rollercoaster that starts in your 40s (sometimes earlier).
Perimenopause can last 4-8 years before your periods actually stop. During this time, your estrogen and progesterone levels fluctuate wildly. The symptoms? Hot flashes that wake you drenched at 3am. Mood swings that make you question your sanity. Night sweats, vaginal dryness, and sleep disturbances that no amount of melatonin seems to fix.
Then comes menopause – officially diagnosed after 12 months without a period. But this isn’t just about periods stopping. It’s about your body adjusting to permanently lower hormone levels.
The impact reaches far beyond hot flashes. Your bone density decreases, raising osteoporosis risk. Your cardiovascular protection drops. Even your brain chemistry changes, affecting memory and mood.
The good news? These changes are normal, not pathological. And there are more options than ever to manage symptoms and protect your long-term health.
Factors That Disrupt Hormone Balance

Factors That Disrupt Hormone Balance
Ever wonder why your hormones seem to go haywire despite your best efforts? You’re not alone. Hormonal imbalances don’t just happen randomly – specific triggers can throw your body’s delicate chemical messengers out of whack.
A. Lifestyle Contributors: Stress, Poor Diet, and Lack of Sleep
Your daily habits pack a serious punch when it comes to hormone health. Chronic stress floods your system with cortisol, which can block progesterone receptors and create estrogen dominance. That’s why you might notice worsening PMS or irregular periods during particularly stressful times.
What you eat matters tremendously too. Processed foods, excessive sugar, and artificial ingredients disrupt insulin sensitivity and inflammation levels. Meanwhile, skimping on sleep (even just one night of poor sleep) can reduce insulin sensitivity by up to 25% and throw your hunger hormones completely off balance.
Try this experiment: track your mood and energy for a week while prioritizing 7-8 hours of quality sleep. The difference might shock you.
B. Medical Causes: Medications, Autoimmune Conditions, and Endocrine Disorders
Sometimes the culprit is hiding in your medicine cabinet. Birth control pills alter your natural hormone production by design. Corticosteroids, certain antidepressants, and even some blood pressure medications can trigger hormonal shifts too.
Autoimmune conditions don’t play nice with your hormones either. Hashimoto’s thyroiditis attacks your thyroid gland, while conditions like lupus can trigger widespread inflammation that disrupts hormone signaling pathways.
Endocrine disorders like PCOS affect roughly 1 in 10 women of reproductive age. With PCOS, your ovaries produce excess androgens, creating a cascade of symptoms from irregular periods to unwanted hair growth.
C. Life Stage Transitions: Puberty, Pregnancy, and Aging
Your body undergoes massive hormonal renovations throughout life. During puberty, estrogen and progesterone levels surge, sometimes causing mood swings that make you feel like you’re riding an emotional rollercoaster.
Pregnancy transforms your hormone landscape entirely. Within the first 8 weeks, estrogen levels climb to 100 times their pre-pregnancy state. After delivery, those levels crash dramatically, which partially explains why 80% of new mothers experience the “baby blues.”
Perimenopause and menopause bring their own challenges as estrogen and progesterone production declines. This transition typically starts in your 40s, though some women notice changes in their mid-30s. The fluctuations explain why you might suddenly experience night sweats, mood changes, or brain fog that seems to come out of nowhere.
Diagnosing Hormone Imbalances: When to Seek Help

A. Recognizing When Symptoms Require Medical Attention
Ever notice how your body sends signals when something’s off? With hormone imbalances, these signals can be easy to brush off as “just stress” or “getting older.” But some symptoms are your body practically shouting for help.
When should you pick up the phone and call your doctor? Here’s the deal:
- Your periods have gone MIA, become super irregular, or suddenly feel like a horror movie
- You’re experiencing hot flashes that disrupt your sleep and daily life
- Mood swings are wrecking your relationships
- Unexplained weight gain that happens despite your best efforts
- Extreme fatigue that doesn’t improve with rest
- Hair loss that seems excessive
- Chronic headaches with no clear trigger
- Persistent insomnia or sleep disturbances
- Severe acne that appears suddenly in adulthood
The rule of thumb? If symptoms interfere with your quality of life for more than two weeks, it’s time to talk to a healthcare provider. Don’t tough it out thinking it’s normal or inevitable. It’s not.
B. Understanding Hormone Testing Options and Procedures
The hormone testing world can feel overwhelming, but it doesn’t have to be. Let’s break down your options:
Blood Tests: The most common starting point. They provide a snapshot of hormone levels at a specific moment.
Saliva Testing: Less invasive and can be done at home. Great for measuring free (active) hormone levels, especially for cortisol patterns throughout the day.
Urine Testing: Comprehensive option that measures hormone metabolites, showing how your body processes hormones.
DUTCH Test: Combines dried urine samples collected throughout the day, giving a fuller picture of hormone fluctuations.
Testing is usually straightforward:
- For blood tests, you’ll visit a lab for a simple blood draw
- For saliva tests, you’ll spit into a tube (often multiple times throughout a day)
- For urine tests, you’ll collect samples according to specific instructions
Many doctors recommend testing at specific times of your cycle for more accurate results. And no, you don’t need to test every hormone under the sun. A good provider will select tests based on your symptoms.
C. Working With Healthcare Providers to Interpret Results
Getting your test results can feel like trying to read hieroglyphics. Those numbers and ranges mean something—but what?
First, understand that “normal” ranges are broad averages, not necessarily optimal for you. What matters most is how your levels correlate with your symptoms.
Finding the right healthcare provider makes all the difference. Consider:
- Conventional doctors (OB/GYNs, endocrinologists) for diagnosing specific conditions
- Functional medicine practitioners for a more holistic approach
- Naturopathic doctors who specialize in hormone health
During your appointment:
- Bring a symptom journal noting patterns and triggers
- Ask specific questions about your results (“Why is this high/low? What does that mean for me?”)
- Discuss treatment options thoroughly before deciding
- Request copies of all your test results for your records
Don’t settle for being dismissed or told your symptoms are “just aging” or “all in your head.” If a provider doesn’t take your concerns seriously, it’s perfectly reasonable to get a second opinion.
Remember, you’re looking for someone who treats you as a whole person, not just a collection of lab values. The right provider will work with you as a partner in restoring your hormone balance.
Effective Strategies to Restore Hormone Balance

Medical Treatments: Hormone Replacement Therapy and Medications
When your hormones are completely out of whack, sometimes you need more than just lifestyle tweaks. That’s where medical treatments come in.
Hormone Replacement Therapy (HRT) is a common option for women experiencing menopause symptoms. It works by replacing the estrogen your body no longer makes. Some women swear by it for hot flashes and night sweats, while others find it helps with mood swings and vaginal dryness.
Bioidentical hormones are another approach. These are chemically identical to the hormones your body produces. Many women prefer them because they’re more “natural,” though the FDA doesn’t always regulate them as strictly.
For specific conditions like PCOS, medications like metformin can help regulate insulin levels, which indirectly balances hormones. Birth control pills are often prescribed to regulate periods and hormone levels for various conditions.
Here’s what you need to know before jumping into medical treatments:
- Always get comprehensive hormone testing first
- Discuss your complete health history with your doctor
- Ask about potential side effects (they exist and matter!)
- Consider starting with the lowest effective dose
- Schedule regular follow-ups to monitor your response
Remember that what works for your best friend might not work for you. Your hormone puzzle is unique, and finding the right medical solution often takes time and patience.
Natural Approaches: Diet, Supplements, and Herbal Remedies
Food isn’t just fuel—it’s information for your hormones. What you eat directly impacts how your hormones behave.
First up, ditch the processed foods and sugar. They’re hormone chaos creators. Instead, focus on:
- Healthy fats like avocados, olive oil, and fatty fish (your hormones are made from these!)
- Cruciferous veggies like broccoli and cauliflower (they help metabolize estrogen)
- Fiber-rich foods that support gut health (where hormone metabolism happens)
- Quality proteins that provide amino acids for hormone production
Specific supplements can work wonders too. Magnesium helps with PMS symptoms and sleep. Vitamin D is crucial for hormone production. Omega-3s reduce inflammation that can disrupt hormone balance.
As for herbs, adaptogenic herbs like ashwagandha and rhodiola help your body manage stress hormones. Vitex (chasteberry) has been used for centuries to balance female hormones, especially for PMS and irregular cycles.
Seed cycling is gaining popularity—eating specific seeds during different phases of your menstrual cycle to support hormone production naturally.
The beauty of natural approaches? They often address the root causes of hormone imbalance rather than just masking symptoms. But patience is key—natural methods typically take 2-3 months to show significant results.
Lifestyle Modifications for Long-Term Hormone Health
Your daily habits either feed or fight hormone chaos. Small, consistent changes can dramatically shift your hormone health over time.
Sleep isn’t optional for balanced hormones—it’s essential. During deep sleep, your body repairs hormone pathways and clears excess hormones. Aim for 7-9 hours of quality sleep in a cool, dark room.
Stress is perhaps the biggest hormone disruptor. When you’re constantly stressed, your body prioritizes stress hormones over reproductive hormones. Find stress management techniques that actually work for you—meditation, walking in nature, or even just proper breathing can make a difference.
Movement matters tremendously. Exercise helps:
- Increase insulin sensitivity
- Reduce excess estrogen
- Boost mood-enhancing hormones
- Improve sleep quality
But here’s the catch—overtraining can worsen hormone imbalances. For many women, gentle yoga, walking, and strength training work better than high-intensity workouts every day.
Environmental factors play a surprising role too. Common products contain endocrine disruptors that mimic hormones in your body. Swap plastic containers for glass, choose clean beauty products, and filter your water.
Track your cycle to understand your hormone patterns. Notice energy levels, mood, and physical symptoms throughout the month. This awareness helps you work with your hormones rather than against them.
The most powerful approach? Combining these lifestyle modifications with the right medical treatments or natural remedies for your specific situation.
Preventive Measures for Maintaining Optimal Hormone Health

Nutrition Principles for Hormone Balance
Your body speaks through hormones, and what you eat directly impacts what it’s saying. Women juggling busy lives often neglect this crucial connection.
Ever notice how your mood tanks after a sugar binge? That’s your hormones screaming for help. Balance starts with steady blood sugar – think protein with every meal, healthy fats like avocados and olive oil, and complex carbs that don’t send your insulin on a rollercoaster ride.
Cruciferous vegetables aren’t just trendy – they actively help your body metabolize estrogen. Broccoli, cauliflower, and kale contain compounds that support your liver’s detox pathways. Your liver is hormone central station, so treat it right!
Seed cycling isn’t some hippie trend – it works. Flax and pumpkin seeds during the first half of your cycle, sesame and sunflower during the second half. They provide the raw materials your body needs to produce hormones properly.
And please, ditch the processed foods. Those fake estrogens and endocrine disruptors lurking in plastics and preservatives? They’re hormone hijackers.
Exercise Routines That Support Endocrine Function
Hitting the gym like you’re training for the apocalypse? You might be doing more harm than good. Hormone-friendly exercise looks different.
High-intensity interval training (HIIT) packs maximum benefits in minimum time, but limit sessions to 20-30 minutes, 2-3 times weekly. Your adrenals will thank you.
Strength training isn’t optional – it’s essential. Building muscle mass supports insulin sensitivity and growth hormone production. Start with bodyweight exercises if you’re new, then gradually add resistance.
The magic happens in recovery. Without adequate rest between workouts, your cortisol levels stay elevated, throwing other hormones out of whack. Those rest days aren’t laziness – they’re medicine.
Yoga and Pilates deserve special mention for women’s hormone health. The combination of movement, breath work and mindfulness directly impacts your endocrine system. The twist poses specifically massage internal organs, improving circulation to hormone-producing glands.
Stress Management Techniques to Protect Hormonal Health
Chronic stress is your hormones’ worst enemy. Period. When cortisol runs wild, it steals the raw materials needed to make other hormones, creating a domino effect of imbalance.
Meditation isn’t woo-woo – it’s science. Even five minutes daily lowers cortisol levels measurably. Can’t sit still? Try walking meditation or guided apps that make it accessible for beginners.
Sleep hygiene matters more than you think. Your body repairs hormonal pathways during those precious hours. Dark room, consistent schedule, no screens before bed – basic but revolutionary.
Adaptogenic herbs like ashwagandha, rhodiola and holy basil help your body resist stress on a cellular level. They don’t just mask symptoms – they actually improve how your adrenals respond to stressors.
Community and connection are your secret weapons. Meaningful social interaction releases oxytocin, the “love hormone” that counteracts stress. Regular laughs with friends isn’t just fun – it’s hormonal medicine.
Remember: perfect hormone balance doesn’t exist. Your body naturally fluctuates. The goal is resilience – creating systems that support your endocrine function through life’s inevitable challenges.

Achieving hormone balance is not a one-time endeavor but a lifelong journey for women. Throughout this blog, we’ve explored the complex world of female hormones—from understanding their vital functions to recognizing imbalance signs and common hormone-related conditions. We’ve examined how factors like stress, medications, and life stages can disrupt this delicate balance, potentially leading to a range of symptoms from weight fluctuations and fatigue to mood changes and reproductive issues.
The path to hormonal wellness begins with awareness and proactive care. If you’re experiencing persistent symptoms, don’t hesitate to consult with a healthcare provider for proper diagnosis and treatment options. Remember that many hormone imbalances can be effectively managed through a combination of medical interventions and lifestyle modifications. By embracing preventive measures—maintaining a healthy diet, engaging in regular exercise, managing stress, and prioritizing quality sleep—you can take meaningful steps toward optimal hormone health and overall wellbeing. Your body deserves this attention and care; after all, balanced hormones contribute significantly to your quality of life at every age and stage.

